What is Eclampsia and Preeclampsia: Causes, Diagnosis, Prevention, Signs, Symptoms, and Management
What is Preeclampsia?
Preeclampsia is a pregnancy-related condition characterized by high blood pressure and often proteinuria (excess protein in the urine). It typically occurs after 20 weeks of pregnancy but can also develop postpartum. If untreated, preeclampsia can lead to serious, even fatal, complications for both mother and baby.
What is Eclampsia?
Eclampsia is a severe progression of preeclampsia, characterized by the onset of seizures in a woman with preeclampsia. Eclampsia can lead to serious complications including coma and death if not promptly treated.
Causes
- Placental abnormalities: Issues with the development and function of the placenta.
- Immune system disorders: Abnormal immune responses to pregnancy.
- Genetic factors: Family history of preeclampsia or eclampsia.
- Pre-existing conditions: Chronic hypertension, diabetes, kidney disease, and obesity.
Diagnosis
- Blood pressure monitoring: Regular checks for high blood pressure.
- Urine tests: Checking for proteinuria.
- Blood tests: Assessing liver function, kidney function, and platelet count.
- Fetal monitoring: Checking the baby's growth and health.
Prevention
- Regular prenatal care: Early and consistent prenatal visits for monitoring.
- Healthy lifestyle: Maintaining a balanced diet, regular exercise, and managing weight.
- Managing pre-existing conditions: Keeping conditions like hypertension and diabetes under control.
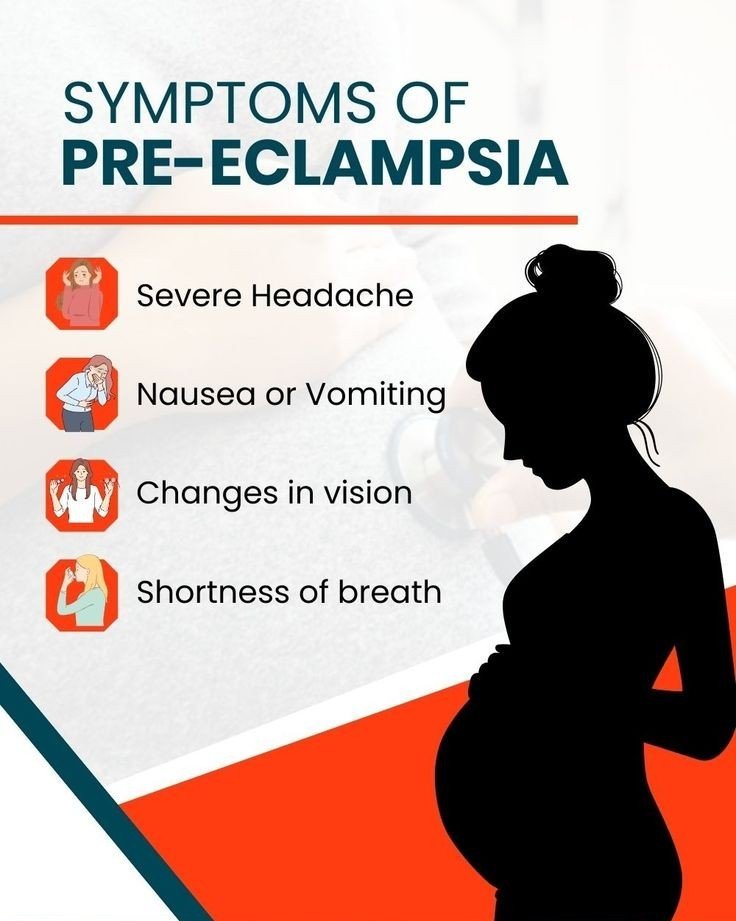
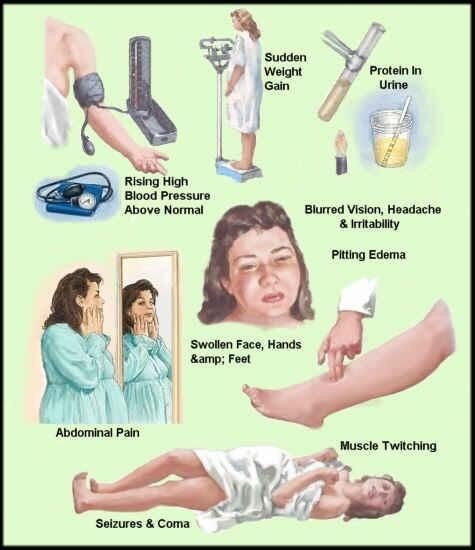
Signs and Symptoms
Preeclampsia:
- High blood pressure
- Proteinuria
- Severe headaches
- Visual disturbances (e.g., blurred vision, seeing spots)
- Upper abdominal pain
- Nausea or vomiting
- Swelling (edema), especially in the face and hands
Eclampsia:
- Seizures
- Loss of consciousness
- Severe headache
- Severe abdominal pain
Management
Preeclampsia:
- Monitoring: Close observation of mother and baby.
- Medications: Antihypertensives to control blood pressure and corticosteroids to help baby's lung development if early delivery is necessary.
- Delivery: Often the only definitive treatment, particularly if the condition worsens.
Eclampsia:
- Seizure management: Immediate medical intervention to control seizures.
- Blood pressure control: Intravenous antihypertensive medications.
- Delivery: Prompt delivery of the baby, regardless of gestational age, to protect the health of the mother.

Frequently Asked Questions
Q1: What are the warning signs of preeclampsia?
A1: Warning signs include high blood pressure, severe headaches, visual disturbances, upper abdominal pain, and significant swelling.
Q2: How is preeclampsia treated during pregnancy?
A2: Treatment involves close monitoring, medications to manage blood pressure, and possibly early delivery if the condition is severe.
Q3: Can preeclampsia be prevented?
A3: While it cannot be entirely prevented, regular prenatal care, a healthy lifestyle, and managing pre-existing conditions can reduce the risk.
Q4: What are the risks of eclampsia?
A4: Eclampsia poses serious risks including seizures, coma, and death if not treated promptly. It also increases the risk of preterm delivery and complications for the baby.
Q5: Is eclampsia common?
A5: Eclampsia is relatively rare, affecting about 1 in 2,000 to 3,000 pregnancies in developed countries.
Q6: What happens after a diagnosis of preeclampsia?
A6: After a diagnosis, the healthcare provider will monitor the mother and baby closely, manage blood pressure, and plan the timing and method of delivery to ensure the best outcomes.
Q7: Can preeclampsia affect future pregnancies?
A7: Yes, women who have had preeclampsia are at higher risk of developing it in future pregnancies. It's important to discuss this with a healthcare provider for proper management in subsequent pregnancies.


You must be logged in to post a comment.